The link between JIA and eye inflammation (uveitis) has been known for about a century. Unlike other forms of uveitis, the eye of an affected JIA patient is often normal appearing & does not appears inflamed. The insidious onset of ocular inflammation can result in significant problems if diagnosis and treatment are delayed.
Uveitis refers to inflammation of the iris, ciliary body and/or choroid. In JIA the iris and ciliary body are affected primarily (iridocyclitis). Up to 20% of children with JIA develop ocular disease, making it the #1 cause of uveitis in children.
Cataracts, glaucoma, band keratopathy and loss of vision can all occur as a result of untreated iridocyclitis. One or both eyes can be affected. A vision screening or direct ophthalmoscopy is not adequate to detect intraocular disease. Only a careful slit-lamp examination can detect the signs of iridocyclitis.
JIA subtypes
Systemic-onset JIA patients rarely develop ocular disease (<2%). Polyarticular (many joint) onset patients have a 7%-37% chance of developing uveitis (representing 10% of those with eye disease). Pauciarticular children (few joints) are especially at risk & represent 90% of JIA uveitis cases. They are most commonly female, with an onset between ages 2 and 5 years. Infrequently uveitis can precede the arthritis; usually it follows the arthritis within 5-7 years (highest risk the first 4 years). Eye disease activity does not have to parallel systemic disease activity. Up to 80% of affected patients are ANA positive (a blood test). The differential should include Lyme disease.
Disease course- asymptomatic & insidious. 1/4 have an excellent prognosis; 1/4 have unremitting inflammation; 1/2 have a relapsing & remitting course.
Treatment- the main form of treatment is topical steroids. Chronic topical steroids have risks (cataracts, glaucoma) which need to be monitored closely. Dilating drops are sometimes needed as well. Less commonly, periocular or systemic steroids are needed to control the inflammation. When chronic treatment is needed Methotrexate is often used. More recalcitrant cases may require TNF-inhibiting anti-inflammatory medications such as Humira or Remicade.
Screening- on a regular basis is crucial, since many affected patients are asymptomatic. Initial exam should occur within 6 weeks of diagnosis. The frequency of screening is dependent on JIA subtype and ANA status. Subtype is determined by the systemic features and the number of joints involved during the first six weeks of the illness.
Pauci (4 or fewer) Poly (5 or more) Systemic (rash and spiking fevers)
Screening visits will vary between every 3-12 months, depending on the various factors. The highest frequency screening, for example, would occur in a young, +ANA, pauciarticular, newly diagnosed JIA patient.
Summary- JIA iridocyclitis can cause significant ocular morbidity- up to 40% of uveitis cases (often in an insidious fashion). Untoward outcomes can be minimized by careful screening, follow-up & treatment. A multi-disciplined team approach offers the best chance for prompt disease detection, maximal therapeutic results and minimal medication induced side effects.
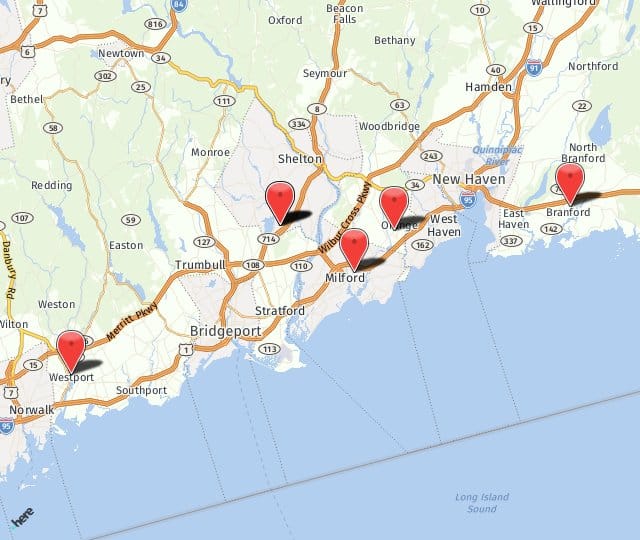
Post by Darron A. Bacal, MD, FAAP. Dr. Bacal is a specialist in Pediatric Ophthalmology and Adult Strabismus. For more information about treatment of ocular inflammation, or any of the services we offer, contact us at any of our 4 offices in Milford, Orange, Branford, or Shelton. We’re looking forward to hearing from you soon.